Causes and Symptoms of Ankle Sprains

Ankle sprains, a prevalent issue, often occur unexpectedly during everyday activities or dynamic pursuits, like sports. The injury typically results from sudden twists or impacts on the foot, causing the tearing of ligaments. In severe cases, a distinctive popping sound or sensation may accompany the tearing of ligaments, serving as a clear indicator of an ankle sprain. Activities such as walking on an uneven surface or stepping off a curb may result in a sprained ankle. Engaging in sports with abrupt movements, like basketball, tennis, football, soccer, and trail running, heighten the risk of ankle sprains. Pain is a common symptom of a sprain, varying in intensity from mild discomfort to intense throbbing. Tenderness around the affected area indicates inflammation and potential ligament damage. Swelling is a natural response to injury, and managing it promptly can aid in reducing overall discomfort. Individuals with sprained ankles may also experience a sense of instability or weakness in the affected ankle, making weight-bearing challenging. Additionally, bruising may occur as blood vessels break due to the injury, leading to discoloration around the affected area. If an ankle sprain is suspected, it is suggested that you make an immediate appointment with a podiatrist for a thorough exam, which may include imaging tests, and an appropriate treatment plan.
Although ankle sprains are common, they aren’t always minor injuries. If you need your ankle injury looked at, contact the foot specialists from Spartan Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains are the result of a tear in the ligaments within the ankle. These injuries may happen when you make a rapid shifting movement while your foot is planted. A less common way to sprain your ankle is when your ankle rolls inward while your foot turns outward.
What Are the Symptoms?
- Pain at the sight of the tear
- Bruising/Swelling
- Ankle area is tender to touch
- In severe cases, may hear/feel something tear
- Skin discoloration
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
In many cases, the RICE method (Rest, Ice, Compression, and Elevate) is used to treat ankle sprains. However, you should see a podiatrist to see which treatment option would work best with your injury. In severe cases, surgery may be required.
It is important to ask your doctor about rehab options after you receive treatment for your injury. Stretching, strength training, and balance exercises may help the ankle heal while also preventing further injury.
If you have any questions, please feel free to contact our offices located in Battle Creek, and Marshall, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankle Sprains
Ankle sprains occur when ligaments that support the ankle stretch beyond their limits and tear. These types of injuries are very common and can occur in people of all ages. Sprains may range from mild to severe, depending on how much damage is done to the ligaments. If a sprain goes untreated, a more severe sprain may occur which can further damage the ankle. Repeated ankle sprains can lead to chronic ankle pain.
There are some risk factors that can increase your risk of suffering a sprained ankle. Those who participate in sports, walk on uneven surfaces, have a prior ankle injury, are in poor physical condition, or wear improper shoes are more likely to get a sprained ankle.
There are a few symptoms to look out for if you suspect you are suffering from a sprained ankle. Some common symptoms are swelling, bruising, tenderness, and instability of the ankle. In cases where the tearing of the ligaments is severe, there may be a “popping” sound when the strain occurs.
The RICE method is proven to be effective in treating ankle sprains. RICE stands for Rest, Ice, Compression, and Elevation. Rest is important for treatment, especially within the first 24 to 48 hours. You should also ice your sprained ankle for the first 48 hours for 20 minutes at a time. A small piece of cloth should be placed between the ice and the affected area. For the compression step, you should wear a brace that is snug, but not too tight that it cuts off circulation. When choosing a brace, be sure to choose one that is suitable for the type of ankle sprain you have. Lastly, you should elevate your foot above the heart as often as possible.
After you treat a sprain, you should go through rehabilitation to prevent the injury from occurring again. There are three phases to the rehab process. The first phase involves resting, protecting, and reducing the swelling of the injury. The second phase consists of restoring the ankle’s flexibility, range of motion, and strength. The third phase consists of slowly returning to activity and maintenance exercises.
If you suspect you have an ankle sprain, you shouldn’t hesitate to consult with your podiatrist. Your podiatrist will be able to give you a proper diagnosis and a suitable treatment option for your condition.
Mobility Challenges for People With Osteoarthritis of the Feet

Mobility can be significantly impacted in individuals with osteoarthritis of the feet. Osteoarthritis is a common joint condition characterized by the breakdown of cartilage, which cushions the joints. When it affects the feet, it can lead to several mobility-related challenges. The pain and stiffness associated with osteoarthritis can make it difficult to walk and move comfortably. Simple activities like standing up, walking short distances, or climbing stairs may become painful and challenging. The loss of joint flexibility in the feet can also affect balance, increasing the risk of falls and further hindering mobility. Osteoarthritis can alter the natural alignment of the feet, leading to abnormal walking patterns and gait disturbances. Additionally, individuals with foot osteoarthritis may become less physically active due to discomfort, which can contribute to overall deconditioning and reduced mobility. Managing osteoarthritis of the feet often involves a combination of treatments, including pain management, orthotics, assistive devices, and lifestyle modifications. When severe and more conservative treatments do not work, surgery may be needed as an intervention. If you suffer from osteoarthritis in your feet and movement is hard, it is suggested that you make an appointment with a podiatrist to discuss treatment that may help you to resume pain-free living.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact the foot specialists from Spartan Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a joint disorder that involves the inflammation of different joints in your body, such as those in your feet. Arthritis is often caused by a degenerative joint disease and causes mild to severe pain in all affected areas. In addition to this, swelling and stiffness in the affected joints can also be a common symptom of arthritis.
In many cases, wearing ill-fitting shoes can worsen the effects and pain of arthritis. Wearing shoes that have a lower heel and extra room can help your feet feel more comfortable. In cases of rheumatoid arthritis, the arch in your foot may become problematic. Buying shoes with proper arch support that contour to your feet can help immensely.
Alleviating Arthritic Pain
- Exercises that stretch the foot can prevent further pain and injury and increase mobility
- Most of the pain can be alleviated with anti-inflammatory drugs, heat, and topical medications
- Massages can help temporarily alleviate pain.
It is best to see your doctor for the treatment that is right for your needs and symptoms. Conditions vary, and a podiatrist can help you determine the right method of care for your feet.
If you have any questions, please feel free to contact our offices located in Battle Creek, and Marshall, MI . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Arthritic Foot Care
During your lifetime, you will probably walk about 75,000 miles, which is quite a lot of stress to put on your feet. As you get older, the 26 bones and 30 joints in each of your feet will lose flexibility and elasticity. Your foot’s natural shock absorbers will wear down as well. Having arthritis added to this mix only makes matters worse. Your joints will become distorted and inflamed, which is why arthritic foot care needs to be something to think about every day.
When dealing with arthritis, having additional foot complications, such as bunions, hammertoes, or neuroma, can be a serious detriment. To avoid these, buy well-fitting shoes with a lower heel and good support. Arthritis causes you to lose your arch, so having shoes with good arch support is also highly recommended.
Aside from getting good arch support, the shoes need to fit comfortably and properly as well. A good place to start is by leaving a finger width between the back of the shoe and your foot to gauge proper size. It is also helpful to have a square or rounded toe box in the front to provide even more comfort. Another thing to look for is a rubber sole that can provide a cushion and absorb shock as you walk. This adds flexibility to the ball of your foot when you push off your heel to walk.
Exercise is another key aspect of arthritic foot care. Exercise not only strengthens and stretches your muscles and joints, but helps to prevent further injury and pain as well. Stretching the Achilles tendon, the tendon located in the back of your heel, will give you added mobility and reduce pain due to stress. Another thing you can do is massage your feet, kneading the ball of your foot as well as your toes from top to bottom.
Stretching the Achilles tendon is a simple exercise that you can do at home anytime. Lean against the wall with your palms flat against the surface while placing one foot forward, towards the wall, and one foot behind you. Bend your forward knee towards the wall while keeping your back knee locked straight, and make sure both your heels are completely touching the ground at all times. This will stretch your Achilles tendon and calf muscles as well. You will feel the stretch almost immediately. You can also stretch your toes in a couple ways. One involves taking a rubber band and wrapping it around both your big toes while your heels remain together. Then, pull them apart to stretch your big toe. You can also place a rubber band around all the toes of one of your feet. Then, try to separate each individual toe, stretching them all.
A final step you can take to help your arthritis is taking non-steroid, non-inflammatory drugs or topical medicines with capsaicin. Unfortunately, there is no complete way to remove all of your arthritic pain. However, following some of this advice can go a long way in staying as pain-free as possible.
Diabetic Foot Ulcers

The main cause of foot ulcers in diabetic patients is often minor injuries happening when they cannot feel their feet properly. This happens due to a condition called peripheral sensory neuropathy. In simpler terms, it means their nerves do not work well, making them less sensitive to pain or injuries. Along with this, deformities in the foot shape and occasional trauma can play a role in causing foot ulcers. Additional factors in foot ulcer formation include calluses, swelling, and problems with blood circulation to the lower legs and feet. Neuropathy seems to involve various chemical processes and high blood sugar levels. Controlling blood sugar is vital in preventing neuropathy and foot ulcers. If you have diabetes and are experiencing foot ulcers, it is strongly suggested that you visit a podiatrist for immediate care.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with the foot specialists from Spartan Podiatry. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our offices located in Battle Creek, and Marshall, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
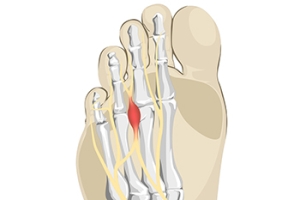
What Causes Morton’s Neuroma?
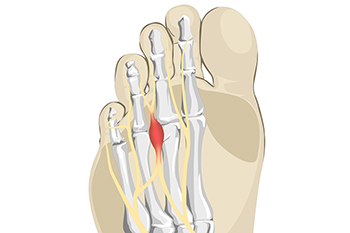
Morton's neuroma is a painful condition that affects the ball of the foot, typically between the third and fourth toes. It is caused by the thickening or enlargement of the tissue around a nerve leading to the toes. Several factors contribute to the development of Morton's neuroma. Wearing tight, narrow, or high-heeled shoes can compress the toes and increase pressure on the nerve, leading to irritation and inflammation. Additionally, individuals with certain foot deformities, such as high arches or flat feet, are more prone to developing Morton's neuroma because these conditions can alter the distribution of weight and pressure on the nerves. Engaging in activities that involve repetitive stress on the forefoot, like running or activities that require tight footwear, can contribute to the development of this condition. A foot injury or trauma can lead to the formation of scar tissue around the nerve, which can then become irritated and inflamed. If you experience symptoms associated with Morton's neuroma, such as pain, numbness, or a burning sensation in the ball of your foot, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact the foot specialists of Spartan Podiatry. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Battle Creek, and Marshall, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
The Importance of Addressing Foot Pain

Foot pain, though often dismissed as a temporary inconvenience, should never be ignored, as it can signify underlying issues that demand attention. Our feet, the foundation of our mobility, are intricate structures comprising bones, joints, muscles, and ligaments. Persistent pain may indicate conditions such as plantar fasciitis, arthritis, or tendinitis, which can worsen without intervention. Ignoring foot pain can lead to altered gait patterns, placing undue stress on other joints and potentially causing a domino effect of discomfort. Moreover, certain foot pain could be a symptom of systemic conditions like diabetes or circulatory issues, requiring timely medical intervention. Chronic foot pain may impact one's quality of life, hindering daily activities and diminishing overall well-being. By recognizing the significance of foot pain and seeking professional evaluation, individuals can safeguard the essential role their feet play in maintaining an active and healthy lifestyle. If you have any type of foot pain, it is suggested that you are under the care of a podiatrist who can provide you with effective relief methods.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with the foot specialists from Spartan Podiatry. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Battle Creek, and Marshall, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.